NIST
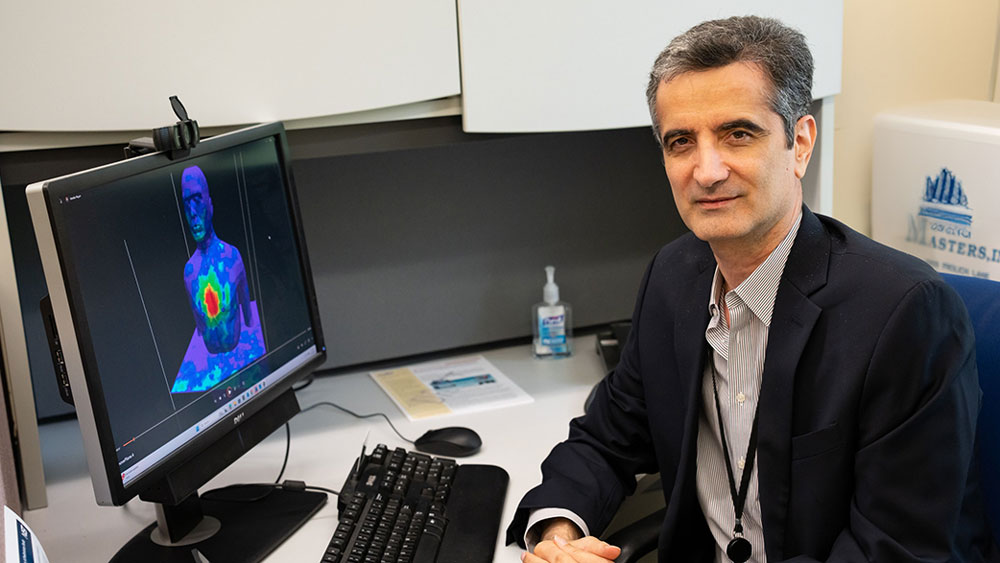
NIST researcher Kamran Sayrafian developed a computational model of the lungs with different levels of excess fluid. The long-term goal is to develop a device that could alert the patient or medical provider when it detects pulmonary edema in the user’s lungs.
A few years ago, I heard on the news that many people were being hospitalized with a condition of excess fluid in the lungs, called pulmonary edema. It’s common in elderly patients. Pulmonary edema is dangerous and can lead to breathing difficulties and lung failure. Because it has the potential to develop suddenly, it can be a serious medical emergency.
|
ADVERTISEMENT |
As a NIST researcher interested in the application of technology in healthcare, I wondered: Is there a way to monitor this condition at home with a simple wearable device?
Specifically, I was curious if the excess fluid in the lungs affects the electrical properties of the lung’s tissues in a way that can be sensed through radio frequency waves with a wearable device. The idea was to put a pair of wearable sensors on the patient’s chest and back. The devices would connect wirelessly through the lungs to monitor the change in the amount of liquid.
…
Add new comment