
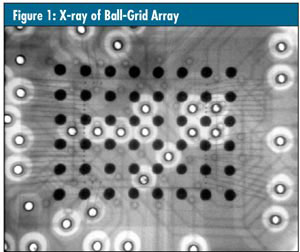
Real-time X-ray inspection systems have been used in quality assurance applications for more than 25 years. In electronics manufacturing, for example, X-ray inspection ensures the registration of drilled holes to internal pads of multilayer printed circuit boards. In electronic assembly applications, X-ray inspection ensures the quality of hidden solder bonds of surface-mounted components such as ball-grid arrays, as seen in figure 1 below.
Now real-time X-ray inspection is becoming an important tool for ensuring the quality of many medical devices. These devices incorporate a diversity of materials, including polymers, rubbers, steel, titanium, ceramics, and glass. Real-time systems employ fluoroscopic imaging devices to display the device’s X-ray image in a video format.
There’s a problem, however, and that’s the limited resolution exhibited by the commercial fluoroscopic and digital imaging devices used by most manufacturers. With limited resolution, the systems are unable to magnify the “shadow” image optically. To compensate, system manufacturers have employed increasingly smaller focal spot sources to achieve increased geometric magnification.
…
Comments
Add new comment