 |
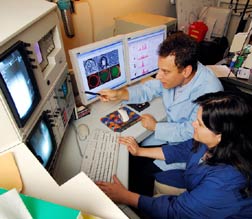
Researchers Mark Prausnitz and Robyn Schlicher use a confocal microscope to study cells whose membranes have been opened by the application of ultrasound. Georgia Tech Photo: Gary Meek |
Researchers have shown how ultrasound energy can briefly open a door in the protective outer membranes of living cells to allow entry of drugs and other therapeutic molecules and how the cells can quickly close the door themselves. Understanding this mechanism could advance the use of ultrasound for delivering gene therapies, targeting chemotherapy and administering large-molecule drugs that cannot readily move through cell membranes.
…
Add new comment