NCQA Evaluates Patient-Centered Medical Homes
The National Committee for Quality Assurance has launched a new version of its Physician Practice Connections program designed to assess how medical practices are functioning as patient-centered medical homes. The new Physician Practice Connections--Patient-Centered Medical Home (PPC-PCMH) program emphasizes the systematic use of patient-centered, coordinated care management processes.
A medical home is a model of care where each patient has an ongoing relationship with a personal physician who leads a team that takes collective responsibility for patient care. The physician-led care team is responsible for providing all the patient’s health care needs and, when needed, coordinating care across the health care system. A medical home also emphasizes enhanced care through open scheduling, expanded hours, and communication between patients, physicians, and staff.
“The patient-centered medical home has the potential to change the interaction between patients and physicians from a series of episodic office visits to an ongoing two-way relationship,” says Margaret E. O’Kane, NCQA president. “Patients can no longer be silent partners in their care--they are active participants in managing their health with a shared goal of staying as healthy as possible.”
A patient-centered medical home can improve health care quality for all Americans, says John Tooker, executive vice president and CEO of the American College of Physicians. “Through the PPC-PCMH, NCQA is helping physicians understand what functioning as a patient- centered medical home means on a day-to-day basis for their practices and establishing standards to recognize physicians who provide this type of care.”
PPC-PCMH includes nine standards for medical practices to meet, including use of patient self-management support, care coordination, evidence-based guidelines for chronic conditions, and performance reporting and improvement. To be recognized as a patient-centered medical home, practices will need to demonstrate the ability to sufficiently meet the criteria of these standards (i.e., achieve a minimum of 25 points out of 100 to attain the first of three levels of recognition) and specifically pass at least five of the following 10 elements:
• Written standards for patient access and patient communication
• Use of data to show that standards for patient access and communication are met
• Use of paper or electronic charting tools to organize clinical information
• Use of data to identify important diagnoses and conditions in practice
• Adoption and implementation of evidence- based guidelines for three certain chronic conditions
• Active patient self-management support
• Systematic tracking of test results and identification of abnormal results
• Referral tracking using a paper or electronic system
• Clinical and/or service performance measurement, by physician or across the practice
• Performance reporting, by physician or across the practice
Large employers have also embraced the patient-centered medical home concept as a means to deliver higher quality care at lower cost.
Many large health plans, as well as Medicare and Medicaid, are planning demonstration projects to learn more about how practices can become medical homes and the quality and cost advantages of doing so.
For more information, visit www.ncqa.org.
Automation Industry Conference
Adept Technology Inc., a provider of intelligent, vision-guided robotics and global robotics services, will host the Adept Global Conference 2008 in Livermore, California, April 2-4, 2008. The automation conference will feature industry leaders, real-world case studies, live automation demonstrations, and networking with automation leaders.
Presentations will be made by Great Lakes Cheese, Pepperidge Farms, Evergreen Solar, Medical Device Magazine , and the Robotics Industry Association on such topics as automation trends for the food industry, medical and solar automation, and robotics.
“We are very excited to be hosting this event, which will give attendees the opportunity to learn about the latest trends and opportunities in robotics, meet with manufacturers and solution providers alike, and view live demonstrations,” says John Dulchinos, president and chief operating officer for Adept Technology Inc.
For more information, visit www.adept.com/conference.
Do the Math
Last month’s “Do the Math” problem came from the Beacon, a publication of the Coast Guard Auxiliary Association (www.cgauxa.org/beacon/Fall07BEACON.pdf). In the article “We’re Aground,” beginning on page 2, amongst the various methods for lightening a boat, was the statement “If the boat is really stuck, empty the water tanks--one square foot of water weighs 8.3 pounds per gallon.”
Almost everyone spotted that a square foot of anything doesn’t have any weight (a cubic foot does) and that water does in fact weigh approximately 8.3 pounds per gallon, unless it’s salt water and full of bilge gunk, in which case it weighs more. For those of you who care, a cubic foot of water weighs approximately 62.4 pounds. When you’re bailing your foundering boat with a five-gallon bucket, you’re hoisting about 40 pounds per bail.
This month’s winner, randomly chosen from all correct entries, was Wayne Flury. Flury will receive a gold-plated five-gallon bucket suitable for bailing, or a present from woot.com.
This month’s error is easy to spot if you have a lot of time on your hands. Daniel J. Montgomery submitted this long article full of facts and figures in which a very simple mistake occurs. Go to www.mpo-mag.com/articles/2007/11/plan-to-prosper, find the error and send it to us by clicking the feedback link at the bottom of this page. Montgomery wins a fabulous Woot prize for his submission.
Send us your math murder. If we use it, you win a mediocre gift for your effort. Entries must come from news stories, articles, advertisements, or similar widely disseminated material.
 Reducing Health Care Waste Reducing Health Care Waste
A recent book puts the health care industry’s biggest challenges into a fresh and useful perspective.
In Paradox and Imperatives in Health Care: How Efficiency, Effectiveness, and E-Transformation Can Conquer Waste and Optimize Quality (Taylor & Francis Inc., 2007), award-winning writers Jeffrey C. Bauer, Ph.D., and Mark Hagland explain why providers must draw upon internal resources to increase net revenue and to provide the quality of care that payers and consumers demand.
Most hospitals, health systems, and other provider organizations are facing financial peril, the authors contend. Mounting receivables from high-deductible health plans, financially challenged consumers, continuing cuts in Medicare, and a precarious economy suggest that real health care spending has peaked. With operating costs increasing and crucial investments in infrastructure not being made, health care providers must find new ways to survive.
Through numerous case studies, the authors show how successful health care organizations are using performance-improvement tools to produce top-quality services as inexpensively as possible. Bauer and Hagland describe the steps that leaders must take to get the best possible value for the $2 trillion already spent annually on health care in the United States.
The book shows why hospitals and medical groups must methodically respond to new political and economic realities that will not be kind to “business as usual.” It also exposes the abundant waste in health care and illustrates economic concepts for producing top-quality care all the time. The authors explain proven techniques for performance improvement and information technologies used in other industries that were forced to change just to stay in business, and establish that providers’ internal transformation is an essential foundation for all other approaches to health reform.
For more information, visit Productivity Press.
New Metrology Vocabulary Guide
The International Organization for Standardization and its partner, the International Electrotechnical Commission, have published a new metrology vocabulary guide.
The guide strives to create a common metrology vocabulary applicable across all industries, where concepts and terms such as “measurement result,” “measurement error,” and “measurement uncertainty” must be agreed upon if they are to be used in a consistent manner.
ISO/IEC Guide 99 cancels and replaces the second edition of the international vocabulary of basic and general terms in metrology (VIM). It is equivalent to the third edition of the VIM.
The need to cover measurements in chemistry and laboratory medicine for the first time, as well as to incorporate concepts such as those that relate to metrological traceability, measurement uncertainty, and nominal properties, led to this third edition.
ISO/IEC Guide 99 takes for granted that there is no fundamental difference in the basic measurement principles of physics, chemistry, laboratory medicine, biology, or engineering. Furthermore, an attempt has been made to meet conceptual needs of measurement in fields such as biochemistry, food science, forensic science, and molecular biology.
For more information, visit www.iso.org.
by Carey Wilson
Where Does It Go?
In a January, 2008, article for National Geographic , author Chris Carroll reminds us that more than 40 years ago, Intel co-founder Gordon Moore observed that because of the speed at which computer software and hardware is developing, at any given time, all of the machines considered state-of-the-art are simultaneously on the verge of obsolescence.
“According to the U.S. Environmental Protection Agency,” writes Carroll, “an estimated 30 to 40 million PCs will be ready for ‘end-of-life management’ in each of the next few years.”
What Carroll means by “end-of-life management” is the scrap heap. And the focus of his article is an examination of where the scrap heaps are, and what goes on when high-tech, electronic waste (e-waste) arrives at them. For the most part, the news is not encouraging.
In an endless ever-growing stream, thousands of tons of e-waste is shipped from the United States, the European Union, and other developed countries to the dumps of developing nations in Africa and Asia, where it is scavenged to recycle the precious (and toxic) metals that allow our high-tech gadgets to function with such efficiency.
At a dump in Ghana, plastic insulation is burned from copper wire over open flames, producing clouds of toxic smoke. The young boys working in this dump also “break copper yokes off picture tubes, littering the ground with shards containing lead, a neurotoxin, and cadmium, a carcinogen that damages lungs and kidneys,” writes Carroll.
Similar scenes occur in China, where “the air near some electronics salvage operations that remain open contains the highest amounts of dioxin measured anywhere in the world. Soils are saturated with the chemical, a probable carcinogen that may disrupt endocrine and immune function. High levels of flame retardants called PBDEs--common in electronics, and potentially damaging to fetal development even at very low levels--turned up in the blood of the electronics workers.”
Carroll closes his article on a hopeful note, describing a high-tech salvaging and recycling machine that harvests the precious components of e-waste without releasing any of its harmful materials into the atmosphere or the ground. So far such machines are rare and expensive, and the majority of e-waste is being recycled in a manner that pits the primordial technology of the open flame against the refined toxins that permeate the devices that sustain our high-tech culture.
For more information, visit www.crserecycling.com.
Easing SOX Compliance
The cost of compliance with the Sarbanes- Oxley Act of 2002 (SOX) has caused many organizations to forget the reason it was passed: to restore integrity in corporate America.
In the aftermath of the Enron and WorldCom scandals, SOX has companies experiencing ups and downs as they seek to enhance public perceptions. The demands of SOX compliance have even caused some organizations to consider privatization to avoid the need to comply. However, ISO 9001- and ISO 14001-certified organizations may find the route to SOX easier.
A Corporate Executive Board survey revealed that 87 percent of CFOs feel that the costs of complying with SOX section 404 exceed the benefits. Established in 2004, the provision requires internal controls over the creation of financial reports. Although it can be challenging to prove a return on spending to comply with regulations, corporate executives realize that they risk prison for failing to do so.
So how do you balance corporate character and a challenging government mandate? Many experts believe that registration to ISO management systems standards offers the best path to renewing integrity. A global community of organizations such as the ANSI-ASQ National Accreditation Board (ANAB) offers increased assurance for businesses through a rigorous assessment process to accredit certification bodies contracted by companies to evaluate their management systems through independent audits.
Management systems standards can provide a foundation for SOX compliance and long-term rewards. Registration to ISO 9001 or ISO 14001 can give organizations a leg up on SOX compliance in various ways that include supporting financial operations and controls, training internal financial auditors to use quality tools, assisting the risk management process, aiding the support process, and developing customer satisfaction measures and objectives for product and service improvement.
A holistic approach to compliance can yield unexpected rewards. According to a recent survey of 180 senior finance executives conducted by CFO Research Services, two out of three respondents said that SOX had helped uncover serious control problems, and they believe that SOX strengthened understanding of their own businesses.
SOX compliance not only helps an organization identify current risks, it also provides a framework to drive the company forward, look ahead five years, and begin making informed decisions on emerging infrastructure needs.
For more information, visit www.anab.org.
Cerulean Outlines Strategies to Cut FDA Compliance Costs
In an article published in the January edition of the Journal of GXP Compliance, “Lean Compliance for Midsized Companies,” Cerulean Associates LLC, a regulatory-compliance consultancy based in Williamsburg, Virginia, outlines five themes to control costs associated with regulatory compliance. These strategies could help biopharmaceutical and medical device executives save at least 1.1 percent of total revenue, or almost $5,400 per employee.
• Simplicity . This means creating a single compliance program under which quality, regulatory, safety, financial controls, electronic security, internal corporate policies, records management, and so forth are managed. This is often the hardest step, but the one upon which all the others rest.
• Rapid prototyping . Determine and embed the minimum controls (e.g., quality, regulatory, etc.) as early as possible in any process, procedure, or system design. Then implement, revise, implement again, and refine and test again--all in 90 days or less.
• Agile risk.Simplify and streamline risk management while building in flexibility and decision-making guidance; in essence, keep the policies and procedures from becoming so rigid that they cannot adapt well to often rapidly changing business climates and priorities.
• Grow knowledge . Based on the old Japanese proverb, “Knowledge without wisdom is like stacking books on the back of a donkey,” the idea here is to develop a strategy to share metrics, trends, decision logic, and results, plus current activities across silos, be they departmental or physical sites.
• Proof. This builds upon good documentation and records retention to use tools and methodologies such as Six Sigma to demonstrate intent to comply and intent to improve. Simplify and prioritize measurement into fewer than 10 metrics that are understandable and actionable by everyone in the organization.
An underlying component of these strategies is that people are encouraged to take a more immediate, hands-on approach toward process improvement by getting emotionally involved. People will figure out a better way to do their jobs and engage in better decision making based on day-to-day knowledge of various tasks and processes. The result is more procedural flexibility, increased capacity for rapid change, and more precise training and management methods.
“The further out into the organization you can push good decision making, reasonable risk taking, and long-term, strategic thinking, the better your compliance and quality programs will be, and thus the lower your costs,” says John Avellanet, Cerulean’s managing director. “Lean compliance is really a systematic strategy to achieve that.”
For more information, visit www.ceruleanllc.com.
Medical Error-Reporting Systems Are Inadequate
Most doctors think that the current systems to report and share information about errors are inadequate, according to a new study funded by the Department of Health and Human Services’ Agency for Healthcare Research and Quality. Instead, they are more likely to rely on informal discussions with their colleagues.
 The study, which appears in the January/February issue of Health Affairs , refers to the exchange of important information regarding medical errors and how to prevent them. The fact that this information is often not shared with the hospital or the health care organization prevents it from being aggregated for analysis and systematic improvement. The study, which appears in the January/February issue of Health Affairs , refers to the exchange of important information regarding medical errors and how to prevent them. The fact that this information is often not shared with the hospital or the health care organization prevents it from being aggregated for analysis and systematic improvement.
“These findings shed light on an important question--how to create error-reporting programs that will encourage clinician participation,” says Carolyn M. Clancy, M.D., AHRQ director. “Physicians say they want to learn from errors that take place in their institution to improve patient safety. We need to build on that willingness with error-reporting programs that encourage their participation.”
Between July 2003 and March 2004, study authors used a 68-question survey to poll a group of more than 1,000 physicians and surgeons to assess attitudes about communicating errors with their colleagues and health care organizations.
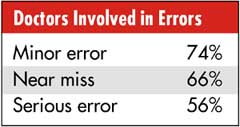
Most physicians reported that they had been involved in some sort of error, from minor to serious, and more than half (54%) agreed with the statement that “medical errors are usually caused by failures of care-delivery systems, not failures of individuals.”
Almost all physicians (95%) agreed that they needed to know about errors in their organization to improve patient safety, and 89 percent agreed that they should discuss errors with their colleagues.
Eighty-three percent said that they had used at least one formal reporting mechanism, most commonly reporting an error to risk management (68%) or completing an incident report (60%). Few physicians believed that they had access to a reporting system that was designed to improve patient safety, and nearly half (45%) did not know if one existed at their organization.
When asked what would increase their willingness to formally report error information, physicians said they wanted:
• Information to be kept confidential and nondiscoverable (88%)
• Evidence that such information would be used for system improvements (85%) and not for punitive action (84%)
• The error-reporting process to take less than two minutes (66%)
• The review activities to be confined to their department (53%)
For more information, visit www.ahrq.gov.
|